Abstract
Treatment of Acute Myeloid Leukemia (AML) should be initiated at the earliest to improve outcomes. The standard induction regimen (3+7) is associated with significant risk of induction mortality, especially in resource limited settings. Hence there is a need to develop risk prediction model for our patient cohorts. Treatment related mortality (TRM) scoring systems developed and used in developed country, mostly for the elderly, may not be directly applicable to population of young adults in developing countries, many of whom have poor general condition and infections at baseline. We developed a multivariate model of induction mortality score in 2019, from a retrospective AML cohort of the Indian acute leukemia research database [INwARD] established by the Hematology Cancer Consortium (HCC). In the present study we have validated the approach and recalibrated the induction mortality score on a multicenter prospective cohort.
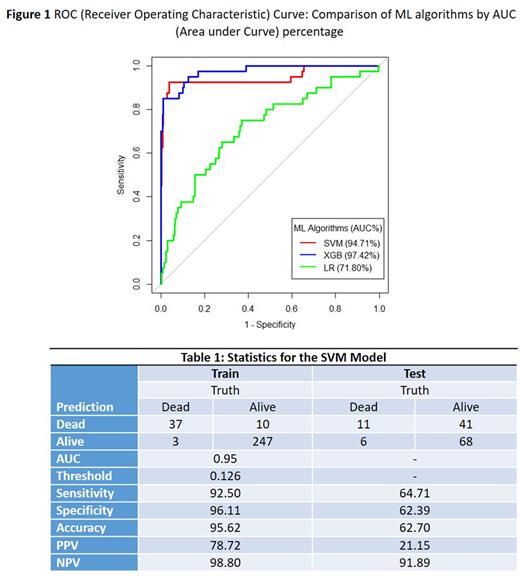
Prospective data for adult AML, for a period of 20 months, starting July 2020 to February 2022, was received from 17 member institutions in a central online data management system. Potential variables that would predict mortality were selected based on clinical and statistical significance. Eleven variables relating to baseline patient and disease characteristics (age, ECOG performance status, duration of symptoms in days, albumin, creatinine, bilirubin, white cell count, platelet, hemoglobin, peripheral blood blast percentage, and presence of infection requiring intravenous antibiotic within one week prior of starting induction), were considered for the predictive model using machine learning (ML) algorithms: Logistic regression (LR), Support Vector Machine (SVM) and eXtreme Gradient Boosting (XGB). Of the various ML algorithms, the best model was chosen based on area under curve (AUC) from the training dataset and validity statistics from the test dataset. We also used the same approach to predict intensive care unit (ICU) admission. R software was used to analyze the data.
Of the 779 treated cases during the study period, 438 received intensive induction, '3+7' being the most common regimen in 80%. The median age of this cohort was 37 years (IQR 28, 46), male to female ratio 1.2. European Leukemia Net (ELN) risk group was good in 31.3 % (n= 137), intermediate in 44% (n=192), high in 13.7% (n=60), and unknown in 11% (n=48). Complete remission was attained in 56.3%. Overall induction mortality was 13.0%, ranging from 7.1% to 40% across different centers. Infection was the most common cause of death in 52%. For predicting induction mortality using 11 covariates, SVM provided the best threshold as 0.126, with an AUC of 94.71%, sensitivity (92.50%), and specificity (96.11%). A comparison of the ML algorithms is shown in Fig 1 and statistics for the SVM model in Table 1. ICU admission was observed in 22.8%; a cut-off threshold of 0.231, with an AUC of 93.3% in the SVM model predicted ICU admission with sensitivity of 93.15% and specificity of 89.7%.
Induction mortality prediction score developed in a retrospective cohort was effectively applied to contemporary prospective data from major centers across the country, with diverse resources and patient profiles. Thus, we have validated the machine learning approach of predicting induction mortality with variables relevant to regional clinical settings including baseline infection. The SVM model predicted the risk of both induction mortality as well as morbidity with high accuracy. An online calculator is being developed to help clinicians use this score in regular practice for guiding treatment intensity as per an individual patient's risk and in directing appropriate resource utilization. Further, the approach of risk-adapted induction intensity, especially for young adult AML, based on the score adjusted to center-specific prevalence of mortality rates, is under consideration for a prospective clinical trial.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal